In today’s fast-paced healthcare environment, Electronic Health Records (EHR) software has become a cornerstone of modern medical practice. This innovative technology replaces traditional paper-based records, offering a centralized, digital platform for storing and managing patient information. From medical histories and lab results to prescriptions and treatment plans, EHR software ensures that vital data is just a click away.
Unlike bulky and error-prone paper records, EHR systems enhance accuracy, improve efficiency, and streamline communication between healthcare providers. They enable seamless data sharing, reduce the risk of misplaced files, and support better decision-making through features like real-time updates and clinical decision support.
This article aims to demystify EHR software, providing a clear understanding of its features, benefits, and role in transforming healthcare. Whether you’re a healthcare professional, a tech enthusiast, or someone curious about how technology is reshaping patient care, this guide will equip you with the basics of EHR and its far-reaching impact.
What is Electronic Health Records (EHR) Software?
Electronic Health Records (EHR) software is a digital solution designed to manage and store comprehensive patient information in a secure and accessible manner. It encompasses everything from medical histories and test results to treatment plans and billing information, serving as a centralized hub for healthcare data.
EHR systems are built to go beyond simple record-keeping. They are interactive tools that provide healthcare providers with clinical decision support, enabling more precise diagnoses and better-coordinated care.
EHR vs EMR: What’s the Difference?
It’s common to confuse Electronic Health Records (EHR) with Electronic Medical Records (EMR). While both are digital systems for storing patient data, they serve different purposes:
EMR (Electronic Medical Records):EMRs are essentially digital versions of paper charts. They focus on recording a patient’s treatment history within a single healthcare provider’s practice.
EHR (Electronic Health Records):EHRs, on the other hand, are designed for interoperability. They facilitate the sharing of patient data across multiple healthcare providers and systems, offering a more comprehensive view of a patient’s medical history.
For example, if a patient visits a general physician and is later referred to a specialist, an EHR allows seamless access to the patient’s records, unlike EMRs, which are confined to the originating provider.
Understanding these distinctions helps highlight why EHR software is critical for modern, collaborative healthcare. It’s not just about digitizing records—it’s about transforming how information is shared and utilized to enhance patient care.
Key Features of EHR Software
Electronic Health Records (EHR) software is equipped with a range of features designed to streamline healthcare workflows and improve patient care. Here are the key functionalities that make EHR software indispensable in modern healthcare:
1. Centralized Patient Records
EHR software consolidates all patient information in one place, including medical history, allergies, medications, test results, and treatment plans. This centralization ensures healthcare providers have quick and easy access to accurate patient data.
2. Interoperability
One of the standout features of EHR software is its ability to integrate with other systems, such as labs, pharmacies, imaging centers, and insurance providers. This interoperability allows for seamless sharing of patient information across multiple healthcare providers and institutions.
3. Clinical Decision Support (CDS)
EHR systems often include decision support tools that assist healthcare providers in diagnosing conditions, identifying potential medication interactions, and recommending treatment plans based on evidence-based guidelines.
4. Secure Data Sharing
EHR software enables secure sharing of patient information while ensuring compliance with privacy regulations like HIPAA. Advanced encryption and access controls protect sensitive data from unauthorized access.
5. Appointment Scheduling and Billing
Beyond medical data, EHR systems streamline administrative tasks such as scheduling appointments, generating invoices, and managing insurance claims. This integration reduces the need for separate systems and minimizes errors.
6. Patient Portals
Patient portals empower individuals to take an active role in their healthcare by providing access to their medical records, test results, and prescriptions. Patients can also schedule appointments, request medication refills, and communicate with healthcare providers directly through the portal.
7. Real-Time Updates and Alerts
EHR systems provide real-time updates on patient data and send alerts for critical issues, such as abnormal lab results or missed follow-ups, ensuring timely interventions.
8. Mobile Accessibility
Many EHR solutions offer mobile access, allowing healthcare providers to review patient records, update notes, and manage tasks from smartphones or tablets, even when on the go.
9. Data Analytics and Reporting
EHR software can analyze patient data to generate reports on trends, outcomes, and operational efficiency. This feature is particularly useful for improving population health management and identifying areas for practice improvement.
These features collectively make EHR software a vital tool for modernizing healthcare delivery, enhancing efficiency, and improving the overall patient experience.
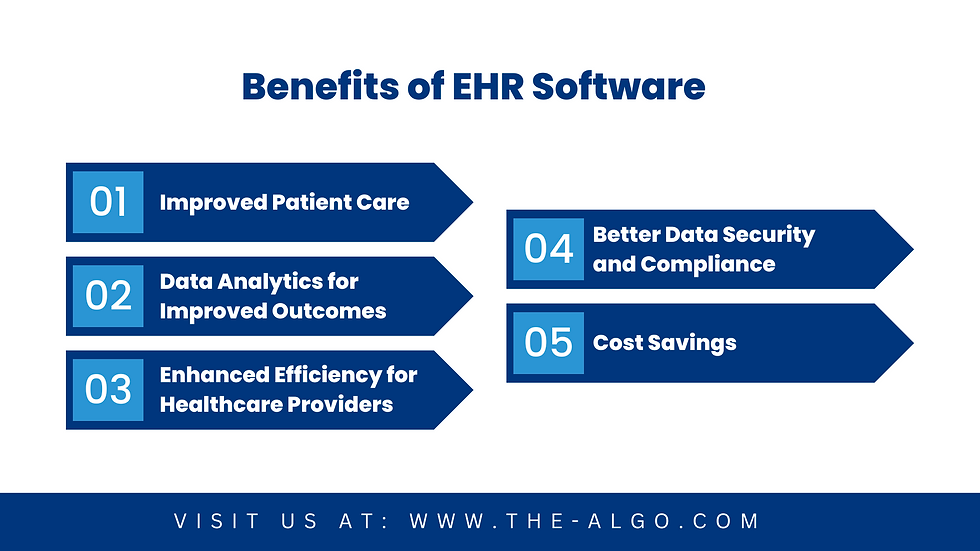
Benefits of EHR Software
The adoption of Electronic Health Records (EHR) software has revolutionized healthcare delivery by offering numerous benefits to both providers and patients. Here’s how EHR software improves healthcare systems:
1. Improved Patient Care
Accurate and Comprehensive Records: EHR systems provide up-to-date and accurate patient information, reducing the chances of errors in diagnosis or treatment.
Better Coordination: With shared access to patient data, multiple healthcare providers can collaborate more effectively, ensuring continuity of care.
Real-Time Alerts: Notifications for critical lab results or potential medication interactions enhance patient safety.
2. Enhanced Efficiency for Healthcare Providers
Streamlined Workflows: EHR software reduces the time spent on manual tasks, such as charting and paperwork, allowing healthcare professionals to focus more on patient care.
Faster Access to Information: Providers can quickly retrieve patient records, improving decision-making speed, especially in emergencies.
Integration of Administrative Tasks: Features like appointment scheduling, billing, and insurance claim management simplify operations and reduce redundancy.
3. Better Data Security and Compliance
Protection of Sensitive Information: Advanced encryption and access controls ensure that patient data is secure and only accessible by authorized personnel.
Regulatory Compliance: EHR software is designed to meet legal requirements, such as HIPAA, safeguarding patient privacy and reducing the risk of penalties.
4. Empowered Patients
Access to Health Information: Patient portals allow individuals to view their medical records, test results, and prescriptions, promoting transparency.
Improved Communication: Patients can use EHR platforms to message their healthcare providers, request appointments, or refill medications conveniently.
Better Engagement: Informed patients are more likely to adhere to treatment plans and take an active role in managing their health.
5. Cost Savings
Reduction in Paperwork: Digital records minimize the costs associated with printing, storage, and retrieval of physical documents.
Fewer Errors: By reducing errors in billing, prescriptions, and diagnoses, EHR systems help avoid costly mistakes.
6. Data Analytics for Improved Outcomes
Population Health Management: EHR software aggregates data to identify trends, track health outcomes, and improve public health strategies.
Performance Insights: Analytics tools provide actionable insights to optimize operational efficiency and clinical effectiveness.
By enhancing patient care, streamlining operations, and enabling better data management, EHR software is a transformative tool that benefits all stakeholders in the healthcare ecosystem.
Challenges in Adopting EHR Software
While Electronic Health Records (EHR) software offers immense benefits, its adoption comes with its own set of challenges. Here are some of the common hurdles faced by healthcare providers:
1. Initial Costs and Implementation
High Upfront Expenses: Implementing an EHR system requires significant investment in software, hardware, and infrastructure upgrades. For smaller practices, these costs can be prohibitive.
Training Requirements: Staff members need extensive training to become proficient with the new system. This can lead to temporary productivity slowdowns and additional costs for training programs.
Implementation Time: Rolling out an EHR system across a healthcare organization can be a lengthy process, causing disruptions to routine workflows during the transition.
2. Resistance to Change
Reluctance Among Staff: Healthcare providers and administrative staff may resist switching from familiar paper-based systems to digital records due to fear of technology, increased workload, or skepticism about the system's benefits.
Overcoming Behavioral Barriers: Addressing this resistance requires clear communication of the benefits, hands-on training, and ongoing support to help staff adapt to the new workflow.
Cultural Shift: Successful adoption often demands a cultural shift within the organization, emphasizing the importance of technology in improving patient outcomes.
3. Data Migration and Interoperability Issues
Transferring Existing Records: Migrating large volumes of data from paper or legacy systems to the new EHR system can be time-consuming and error-prone. Incomplete or inaccurate data transfer can disrupt patient care.
Lack of Standardization: Many EHR systems lack standardized data formats, making it difficult to integrate with other software, such as lab or imaging systems. This creates interoperability challenges.
Vendor Lock-In: Some EHR vendors design their systems to be proprietary, limiting the ability to share data with other providers or systems. This can hinder collaboration and continuity of care.
Addressing these challenges requires careful planning, adequate budget allocation, and a focus on staff engagement and training. By proactively tackling these hurdles, healthcare organizations can ensure a smoother transition to EHR systems and maximize their benefits.
How to Choose the Right EHR Software
Selecting the right Electronic Health Records (EHR) software is crucial for ensuring seamless integration into your healthcare practice and maximizing its benefits. Here are key factors to consider when making your choice:
1. Assess Your Practice’s Needs
Specialization Requirements: Choose an EHR system designed to meet the unique needs of your medical specialty, whether it's pediatrics, cardiology, or general practice.
Practice Size: Consider whether the software is tailored for small clinics, large hospitals, or multi-specialty practices.
Must-Have Features: Identify essential features, such as patient portals, appointment scheduling, and clinical decision support tools, to prioritize your practice's needs.
2. Ease of Use
User-Friendly Interface: A system with an intuitive interface minimizes the learning curve for staff and ensures efficient workflows.
Customizable Templates: Look for software that allows customization of templates to fit your practice's specific workflows.
3. Interoperability and Integration
Seamless Integration: Ensure the EHR software can integrate with existing systems like lab equipment, imaging software, and billing platforms.
Data Sharing Capabilities: Choose a system that supports interoperability with other healthcare providers to facilitate seamless data exchange and coordinated care.
4. Compliance and Security
Regulatory Compliance: Verify that the EHR software adheres to regulations like HIPAA to ensure the privacy and security of patient data.
Data Encryption and Backup: Opt for a system with robust security measures, including encryption, regular backups, and disaster recovery plans.
5. Cost and Scalability
Upfront and Recurring Costs: Evaluate the total cost of ownership, including setup fees, subscription costs, and maintenance expenses.
Scalability: Choose software that can grow with your practice, accommodating increasing patient volumes or additional providers.
6. Support and Training
Vendor Support: Ensure the vendor offers reliable customer support, including troubleshooting, updates, and technical assistance.
Training Resources: Select a vendor that provides comprehensive training programs for your staff to ensure smooth adoption.
7. Reputation and Reviews
Vendor Reputation: Research the vendor’s track record, client testimonials, and industry certifications to assess their reliability.
Peer Recommendations: Consult with other healthcare professionals to learn about their experiences with various EHR systems.
8. Trial Period and Demonstrations
Free Trials: Take advantage of free trials or demonstrations to test the software’s functionality and usability before committing.
Hands-On Evaluation: Involve your staff in the evaluation process to gather feedback and ensure the system meets their needs.
By carefully evaluating these factors, you can select an EHR system that aligns with your practice's goals, enhances efficiency, and improves patient care.
Future Trends in EHR Software
The evolution of Electronic Health Records (EHR) software continues to reshape healthcare. Emerging trends indicate a future where EHR systems become even more intelligent, interoperable, and patient-centric. Here are key developments to watch:
1. Artificial Intelligence and Machine Learning
Predictive Analytics: AI-powered EHR systems will provide insights into patient trends, predict potential health issues, and recommend preventive measures.
Natural Language Processing (NLP): NLP technology will allow providers to dictate notes, which the system can convert into structured data, streamlining documentation.
Clinical Decision Support: AI integration will enhance clinical decision-making by analyzing patient data and offering evidence-based recommendations.
2. Telehealth Integration
Remote Monitoring: EHR systems will increasingly incorporate telehealth tools, enabling healthcare providers to track patients’ health metrics remotely.
Virtual Consultations: Seamless integration with telehealth platforms will allow providers to access patient records during virtual visits, ensuring comprehensive care.
3. Blockchain for Enhanced Security
Secure Data Sharing: Blockchain technology will enable tamper-proof and secure data exchange between providers, ensuring data integrity and privacy.
Patient-Centric Ownership: Blockchain may empower patients to control access to their health data, enhancing transparency and trust.
4. Increased Interoperability
Data Exchange Standards: Adoption of universal standards like HL7 FHIR (Fast Healthcare Interoperability Resources) will improve data exchange across platforms.
Cross-Platform Accessibility: EHR systems will become more compatible with other healthcare technologies, breaking down silos and fostering collaboration.
5. Patient-Centric Features
Enhanced Portals: Future patient portals will offer personalized insights, treatment tracking, and proactive health reminders.
Wearable Device Integration: EHRs will incorporate data from wearable devices, providing a more comprehensive view of patient health.
6. Cloud-Based Solutions
Scalable Infrastructure: Cloud-based EHR systems will offer scalability and cost efficiency, making them accessible to smaller practices.
Real-Time Access: Providers and patients will benefit from secure, anytime-anywhere access to health records.
7. Focus on User Experience (UX)
Simplified Interfaces: Future EHR systems will prioritize user-friendly designs to reduce the cognitive burden on healthcare providers.
Voice-Activated Commands: Voice-enabled EHRs will further simplify data entry and retrieval, boosting productivity.
8. Regulatory Advancements
Global Standards Compliance: Future EHR systems will adapt to evolving regulatory landscapes, ensuring compliance with international and local laws.
Proactive Updates: Vendors will incorporate real-time regulatory updates to keep systems compliant and future-proof.
9. Data Analytics for Population Health
Big Data Utilization: Advanced analytics will help identify public health trends, optimize resource allocation, and improve care delivery on a broader scale.
Personalized Medicine: EHR systems will use patient-specific data to tailor treatments, advancing the field of precision medicine.
By embracing these trends, EHR software will continue to drive innovation in healthcare, improving outcomes for providers and patients alike while setting new benchmarks for efficiency and care quality.
FAQs
1. What is the difference between EHR and EMR?
Electronic Health Records (EHR):EHRs are comprehensive systems that store a patient’s health information across multiple providers and facilities, enabling seamless sharing and coordination of care.
Electronic Medical Records (EMR):EMRs are digital versions of paper charts used primarily within a single healthcare practice, with limited sharing capabilities.
In short, EMRs are practice-specific, while EHRs are designed for interoperability across healthcare organizations.
2. Is EHR software expensive to implement?
Yes, implementing EHR software can be costly due to:
Upfront Expenses: Licensing fees, hardware upgrades, and installation costs.
Training Costs: Educating staff to use the system effectively.
Ongoing Maintenance: Regular updates, IT support, and data storage fees.
However, the long-term benefits, including improved efficiency and reduced paperwork, often outweigh the initial investment.
3. How does EHR software improve patient care?
EHR software enhances patient care in several ways:
Improved Accuracy: Reduces errors by maintaining accurate and up-to-date patient information.
Better Coordination: Facilitates seamless sharing of health data among providers for coordinated care.
Faster Access: Allows healthcare professionals to quickly retrieve patient records, leading to timely and informed decision-making.
Patient Engagement: Features like patient portals empower individuals to take an active role in their healthcare.
4. What should I look for when choosing an EHR system?
When selecting an EHR system, consider:
Ease of Use: A user-friendly interface that minimizes training time.
Customization: Features that cater to your practice’s unique needs.
Interoperability: Ability to integrate with existing systems and share data seamlessly.
Compliance: Adherence to regulatory standards like HIPAA for data security.
Vendor Support: Reliable customer service and training resources.
Scalability: The ability to grow with your practice and adapt to future needs.
By evaluating these factors, you can choose an EHR system that aligns with your operational goals and improves care delivery.

コメント